Updated: August 2022
Table of Contents
GLOSSARY
ALARA
An acronym for As Low As Reasonably Achievable. The radiation exposure to every person should be kept ALARA, taking into account social and economic factors
Absorbed Dose
The quantity of radiation energy absorbed in a unit of mass of material. SI unit: Gray (Gy).
Air Kerma
The sum of the initial kinetic energies per unit mass of all the charged particles liberated by uncharged ionizing radiation in air.
Background Radiation
Natural radiation resulting from cosmic and terrestrial sources. Background radiation does not refer to occupational exposure or sources from medical uses but includes consumer products.
Bremsstrahlung Effect
The creation of X-rays during the slowing down of an electron (or any other charged particle) moving in the strong electric field (e.g.: nucleus field of an atom); this process of X-ray production is called bremsstrahlung from the German phrase “braking radiation”
Characteristic X-rays
X-rays can be created when electrons re-arrange inside of an atom, resulting in a loss of energy of the atom in the form of X-rays. This process of emission of X-rays is “characteristic” of the target atom
Dose see Absorbed, Equivalent, or Effective Dose
Dose Rate
It is the dose received per unit of time (e.g.: gray per hour Gy/h, sievert per year Sv/year)
Dosimeter
A device used to record the dose received by an X-ray user. Personal dosimeters (or radiation badges) are worn at chest or waist levels to record whole-body exposure, or on a finger to record the extremity exposure. Thermoluminescent dosimeters (TLD) are composed of thermoluminescent material chips (i.e. lithium fluoride [LiF]), which record the exposure to ionizing radiation.
Electron Volt (eV)
It is a unit of energy defined as the energy of an electron that has been accelerated through an electric potential of one volt. One electron volt is 1 eV = 1.6 * 10-19 J. Typically the radiation energies associated with X-rays are in order of magnitude of tens thousands of eV: 40-80 keV.
Equivalent Dose
A measurement of the biological effects on a tissue or organ exposed to a specific type of radiation. It is a function of the absorbed dose and depends on the type of radiation absorbed. SI unit: Sievert (Sv).
Effective Dose
A measurement of the whole body dose based on the summation of the equivalent dose received by all organs. Each organ contributes with a tissue-weighting factor. The effective dose has the same units of measure as the equivalent dose (Sv).
Exposure
A measure of X-ray intensity in terms of its ionizing effect in air. SI unit: C/kg.
Failsafe Design
A design in which any failure of safety indicators or components that can reasonably be anticipated causes the production or emission of X-ray to cease.
Filtration
A process using filters made from metal to improve the quality of the image obtained with the x-ray machine.
Genetic Effects
Biological effects from ionizing radiation exposure that are inherited by children from their parents.
Gray
SI unit of absorbed dose is called Gray (Gy). 1 Gy = 1 J/kg
Ionizing Radiation
Radiation with sufficient energy to create ions.
Permit Holder (PH)
Generally, an appointed U of T professor who is in charge of an X-ray source situated on U of T controlled areas.
Photoelectric Effect
When the interaction between a photon and an atom results in total absorption of the photon and the emission of an electron from the atom. This effect is preponderant at low incident photon energies.
Radiation weighting factor
Takes into account the biological effect of each type of radiation on the human body. It is a number between 1 (for beta, gamma and X-ray) and 20 (for alpha or high-energy neutrons) used to calculate the equivalent dose of an organ when the absorbed dose in that organ is known.
Scattered Radiation
When the interaction between a photon and atom results in partial absorption of the photon, the emission of an electron from the atom, and the emission of a scattered photon with lower energy than the incident photon. This effect is also called Compton effect and is preponderant at average incident photon energies.
This term can also be used to describe the X-rays that scatter over and around shielding walls.
Sievert
SI unit for equivalent and effective dose (Sv)
Shield or Shielding
Radiation absorbing material used to reduce the absorbed dose or absorbed dose rate imparted to an object or tissue.
Somatic Effects
Biological effects from ionizing radiation exposure in our lifetime are called somatic effects. Somatic effects may result from acute or chronic doses of radiation.
Tissue Weighting Factor
Takes into account the biological effect of radiation on different organs or tissues of the human body. It is a percent attributed to each organ or tissue from the human body, used to calculate the effective dose when the equivalent doses received by human organs are known.
X-ray machine
An electrically powered analytical device with the primary purpose of producing X-rays to analyze materials or structures.
X-ray source
Any part of a device, in whole or in part that emits X-rays, whether or not the device is an X-ray machine. The primary use of the device may not be the production of X-rays. Examples include electron microscopes or high voltage sources.
X-ray worker
Any person who in the course of his work, business or occupation, is likely to receive a dose of ionizing radiation in excess of the annual dose allowed to the general public.
X-ray source supervisor
An X-ray worker who due to his/her knowledge, experience and training is designated by the permit holder to supervise the safe use of an X-ray source.
X-ray
It is a type of ionizing radiation (maximum energy greater than 5 keV) that is generally produced from machines rather than emitted from radioactive materials. X-rays are made up of photons.
ENVIRONMENTAL HEALTH AND SAFETY (EHS) CONTACTS
Environmental Health and Safety (EHS):
Radiation Safety :
https:/ehs.utoronto.ca/our-services/radiation-safety
X-ray Safety Contacts
Daniel Cardenas, Health and Safety Officer, X-ray Safety Officer, daniel.cardenas@utoronto.ca
University of Toronto X-ray Safety Policy
Preamble
In accordance with its Health and Safety Policy and the general provisions of the Occupational Health and Safety Act of Ontario, the University of Toronto is committed to promoting the health, safety and well-being of its employees, students, visitors, and contractors.
X-ray sources are part of day-by-day university activity. They are present in our research and teaching laboratories, student projects and other activities that incorporate X-ray sources in the educational and research processes. Radiation generated by X-ray sources can cause a wide range of negative health effects when not used in accordance with rules and regulations.
The ALARA (As Low As Reasonably Achievable) concept has been adopted by the UTRPA as the philosophy governing the use of all ionizing radiations. The ALARA principle seeks to keep all doses of ionizing radiation as low as reasonably achievable, social and economic factors being taken into consideration. No practice involving the exposure of patients or X-ray workers to ionizing radiation may take place if there is no benefit to them as a result of carrying out the practice. Radiation exposures must be kept below the statutory limit regardless of the practice. Persons using X-ray equipment should endeavour to keep all radiation exposures as low as possible.
Mandate and Application
The University has the responsibility to ensure that reasonable and adequate controls exist for the safe use of X-ray sources in all U of T controlled areas. Hazard evaluations should be performed, and appropriate engineering and administrative controls should be put in place, before using any X-ray sources.
This X-ray safety Policy applies to areas controlled by the University of Toronto: buildings, structures or open areas, to all employees and students of the University, to occupants of University buildings, and to external organizations that may use or be affected by X-ray sources hazards in such areas.
In the Province of Ontario, the Ministry of Labour, Immigration, Training and Skills Development (referred here as “MOL”) under the Occupational Health and Safety Act, regulates the use of non-medical X-ray sources. The Ministry of Health (MOH), under the Healing Arts Radiation Protection (HARP) Act and the Occupational Health and Safety Act and regulations, regulates the use of medical X-ray machines. X-ray sources that produce X-rays of high energy capable of inducing radioactivity in materials exposed to them are regulated and licensable by the federal government, under the Nuclear Safety and Control Act (NSCA), enforced by the Canadian Nuclear Safety Commission (CNSC).
University of Toronto Radiation Protection Authority (UTRPA)
The UTRPA is responsible for the safe use of all sources of ionizing and non-ionizing radiation (both materials and machines), in all areas under U of T control. The use of X-ray sources and X-ray machines is under the jurisdiction of the UTRPA.
The UTRPA approves the University X-ray sources Safety Program and ensures that all components of the program are adequately implemented. The essential elements of the program are:
- The registration of all X-ray sources used in University controlled areas
- Hazard evaluation of the X-ray sources
- Training of all X-ray sources users
The implementation of these parts of the program relies on University faculty members (Permit Holders/Supervisors) responsible for the use of X-ray sources. The Permit Holders are fully responsible for the safe use of X-ray sources under their jurisdiction. They must ensure that X-ray sources’ users are competent to use X-ray sources safely, that the X-ray sources’ hazard evaluation is performed and that adequate controls are in place, before using the X-ray sources.
Implementation of the X-ray Safety Program
The Radiation Protection Service (RPS) of the Environmental Health and Safety Office has the responsibility of implementing, updating, and auditing the X-ray Safety Program. The Radiation Protection Service will nominate one Health and Safety Officer as the University X-ray Safety Officer (XSO).
The University X-ray Safety Officer has the authority to stop the use of any X-ray sources in the University controlled areas if the health and safety of persons (faculty, staff, students, visitors) or the environment are at risk. The use of those X-ray sources can be resumed only after all control measures are implemented according to the University X-ray Safety Program and upon written approval of the UTRPA.
1. Introduction and Scope
The X-ray Safety Program is intended to assist the University community in the effective control of X-ray hazards.
The basic elements of the control program are:
- X-ray permit system;
- registration of all X-ray machines and X-ray sources;
- requirements for the inspections of X-ray machines and X-ray sources;
- requirements for training and education of X-ray workers;
- requirements for reporting accidents/incidents involving X-ray machines and X-ray workers
- requirements for personal dosimetry;
- requirements for engineering controls;
- requirements for administrative and procedural controls;
- requirements for auditing the implementation and effectiveness of the program.
Scope
This program applies to all X-ray machines and X-ray sources in areas under the jurisdiction of the University of Toronto. Compliance with this program is mandatory for all faculty, staff or students who possess and/or use X-ray sources at the University of Toronto.
2. General
2.1 Generation of X-rays
X-rays are a type of ionizing radiation (maximum energy greater than 5 KeV) that is generally produced from machines rather than emitted from radioactive materials.
Gamma and X-rays are not comprised of physical particles like alpha or beta radiation but are made up of individual packets of energy called photons.
Unlike gamma rays, which are emitted from the nucleus of a radioactive atom, X-rays are emitted when:
- High-speed electrons (or any charged particles) are slowed down or change direction in a strong electric field like the one created by the nuclei (see Bremsstrahlung Effect) of the target materials. These types of x-rays are called continuous because the x-rays emitted during this process have energies ranging from zero to maximum energy. This maximum energy is equal to the energy of the incoming electron.
- Electrons move from a higher to a lower level of energy inside an atom. These types of X-rays are called characteristic X-rays and have a line-type spectrum. Therefore, characteristic X-rays are emitted from the electron shell of an atom.
X-rays can also be emitted as a secondary effect in instruments that use high voltages (on the order of tens of kV) as power sources for other applications.
2.2 X-ray interaction with matter
After X-rays hit matter they interact with the atoms of the matter through various mechanisms by either being absorbed or scattered. The most common interaction of X-rays with matter include:
2.2.1 Photoelectric Effect
The photoelectric effect occurs when an orbital electron absorbs the energy of an incident photon, and the electron is ejected from the atom. The ejected electron can cause ionization and in the process reduces its energy. This effect is more probable to appear when a low-energy incident photon interacts with a high-Z material target.
2.2.2 Compton Scattering
During this type of interaction, the orbital electron absorbs only a part of the energy of the incident photon and as a result, the electron is ejected from the atom. The remaining energy of the incident photon is carried by a scattered photon. This process is also called Compton scattering. This type of interaction is more probable to occur when the incident photon carries intermediate energy. The scattered photon may undergo another scattering process, resulting in another reduction of energy. When X-rays pass through any material, some will be transmitted, some will be absorbed and some will scatter. The proportions depend on the photon energy and the type of material.
2.3 Units for measuring X-ray energy absorbed in matter
2.3.1 Exposure
X-rays can produce air ionization. The exposure measures the electric charge (positive or negative) produced by electromagnetic radiation in a unit mass of air, at standard atmospheric conditions (STP means 0 degrees Celsius and 760 mm Hg of pressure = 1 atm).
In the SI system of units, exposure is measured in the X unit:
1 X unit = 1 C/kg air
where C stands for coulomb, the SI unit for electric charge.
The average energy dissipated to produce a single ion pair in the air is 34 eV. Since the charge of an electron is equal to 1.6 x 10-19 C, an association can be established between an X unit and the energy measured in joules, dissipated in 1kg of air. Hence, one X unit is equivalent to 34 J/kg.
Exposure refers to the effect of X-rays in air. However, it is often used to characterize the intensity of an X-ray source or an X-ray beam.
2.3.2 Air kerma
Charged particles (free electrons and positive ions) produced by X-rays in the air have each a kinetic energy equal to the difference between the energy lost by the X-rays and the electron bound energy in the atom. Air kerma is the sum of all initial kinetic energies of ions produced by X-rays in a unit of mass of air. The SI unit for air kerma is the same as for the absorbed dose (see below).
Even though the air kerma and absorbed dose have the same units they are quite different. When some of the ions escape from the volume of air (if the air volume is small) air kerma is bigger than the absorbed dose. When all the ions produced are absorbed in the air volume, air kerma is smaller than the absorbed dose
2.3.3 Absorbed Dose (D)
Total X-ray energy absorbed per unit of mass of material is measured in Gy. In this case, the definition is not restricted to air but refers to any type of material.
1 Gy = 1 J/kg
The absorbed dose is used to measure the acute effects of radiation.
2.3.4 Equivalent Dose (H)
The equivalent dose (H) is the physical quantity used to measure the long-term biological effects on a specific tissue or organ. H is a function of the absorbed dose and depends on the type of absorbed radiation. If more than one type of radiation is absorbed in tissue, the equivalent dose, H is:
The radiation-weighting factor (wR) for X-ray is 1 but can vary between 1 to 20 for other types of radiation. H is measured in sieverts (Sv).
2.3.5 Effective Dose (E)
The effective dose, also called the whole-body dose, is the sum of the equivalent doses received by all organs. Each organ that was irradiated contributes to the effective dose with a tissue-weighting factor (WT). WT is expressed as a percentage.
E has the same units of measure as the equivalent dose (Sv)
2.4 Radiation measurements
2.4.1 Particle counting instruments
To measure the intensity of an X-ray source or an X-ray beam a particle-counting instrument can be used. In general, the instruments used to measure X-ray intensity are gas-filled type detectors. This type of detector uses the ionization effect of the X-rays. The most common detectors are Geiger-Muller (GM) or ionization chambers. The meter indication of this type of instrument is in counts per minute (cpm) or counts per second (cps). The reading depends on the type of the detector, the detector’s window and dimensions, as well as on the geometry of the measurement process.
2.4.2 Dose measuring instruments
If a gas-filled detector wall is built with tissue-equivalent material, the instrument can measure tissue dose directly. The most used instrument to measure the exposure or the dose generated by an X-ray source has an ionization chamber detector.
2.4.3 Personal dosimeters
The dose received by a person working with or near an open X-ray source can be measured by a personal dosimeter. There are two different types of personal dosimeters: one that indicates the dose received immediately and one that stores the information inside the dosimeter. In the last case, the stored dose is read later.
A personal electronic dosimeter (PED) is an example of the first type. This instrument can indicate the shallow dose (dose received by the surface of the skin up to the depth of 0.007 cm) and the deep dose (dose received by a person up to one cm depth inside the tissue). It can also be set up to alert, through an alarm system, when a certain dose or dose rate is reached.
A few examples of the second type of personal dosimeters are film, a thermo-luminescent dosimeter (TLD), and optically stimulated luminescence (OSL) dosimeter. The X-ray energy is deposited inside the dosimeter’s material and can be read later by a method specific to each type of dosimeter.
2.5 Biological effects
The biological effects of X-rays can be classified as direct or indirect, acute or delayed, and deterministic or stochastic.
When radiation is absorbed in the biological material causing direct damage to the DNA or other parts of the cell, is called direct action. X-rays can break these molecules and the cell can be damaged resulting in cell death or cell function alteration. The altered cells can be repaired or can be transformed. Depending on the level of radiation the cell death or alterations can be dangerous.
When radiation is absorbed in atoms or molecules other than biological material (for example in a water molecule) the interaction can cause an indirect action. Ions and free radicals resulting from these interactions can damage the biological material indirectly.
Among acute effects of skin overexposure to X-rays are erythema (skin reddening), changes in pigmentation, epilation, blistering, necrosis, and ulceration. Radiation exposure of the whole body with doses between a few hundred mSv and 2000 mSv, can generate acute radiation effects like blood changes, nausea, fatigue, vomiting, impotence, loss of hair, etc. Overexposure of the whole body with a dose of 2000 mSv or more, can result in acute hemopoietic, gastrointestinal, and central nervous system radiation syndromes.
Delayed effects of radiation may be due either to a single large overexposure or continuing low-level overexposures to X-rays. Among the delayed consequences of overexposure to X-rays that are of concern are cancer, genetic effects, mental retardation of children who have been irradiated in utero, and cataracts.
Deterministic effects are effects in which a clear connection can be established between the person that suffered overexposure to radiation and the effect. In these cases, there is a causal relationship between dose and effect on a particular individual. A certain minimum dose must be exceeded to cause a deterministic effect. The severity of the deterministic effects increases with the dose. Deterministic effects can be acute or delayed.
If a large population is exposed to radiation, some individuals will develop cancer and/or damages to the reproductive cells resulting in genetic malformation of the offsprings. These types of effects are called stochastic since they appear by chance. The stochastic effects can occur with no threshold dose, and their probability of occurrence increases with an increase in dose received by the population. The stochastic effects are delayed
3. Responsibilities
This section outlines the responsibilities for the implementation of the X-ray safety program within the University.
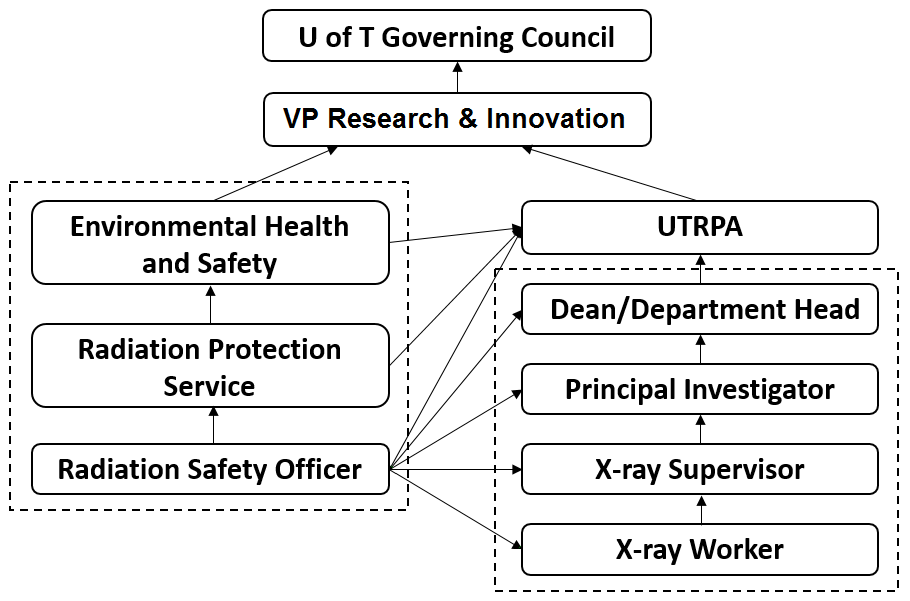
The responsibility chart for X-ray safety on U of T controlled areas is presented below.
Figure 1 – Responsibility for X-ray safety in U of T
3.1 University of Toronto Radiation Protection Authority (UTRPA)
The terms of reference of the UTRPA are outlined in the U of T Ionizing Radiation Policies and Procedures Manual.
The UTRPA’s responsibilities regarding the X-ray sources are:
- To approve the U of T X-ray safety program; periodically assess its effectiveness and recommend changes;
- To establish and maintain standards and guidelines for the safe use of X-ray sources within the University;
- To provide expert advice on X-ray safety hazards;
- To approve the content of the X-ray safety training;
- To review and act on the recommendation of the Director, Research Safety and Compliance, to suspend, restrict or terminate the operation of X-ray sources;
- To report annually to the Vice-President, Research and Innovation, on the operation of the X-ray safety program.
3.2 Radiation Protection Service
The Radiation Protection Service of the Office of Environmental Health & Safety has the following responsibilities within the X-ray safety program:
- To update and present the U of T X-ray safety program for approval of the UTRPA;
- To designate a Health and Safety Officer to serve as the X-ray Safety Officer fulfil the requirements of the X-ray safety program;
- To notify Permit Holders of the X-ray safety program training of all X-ray supervisors/workers under their authority;
- To provide administrative support to the UTRPA regarding the X-ray sources;
- To audit the implementation and effectiveness of this program on an ongoing basis.
3.3 X-ray Safety Officer
The X-ray Safety Officer (XSO) is directed by the Director of the Office of Environmental Health and Safety and UTRPA and is knowledgeable in the evaluation and control of X-ray sources hazards.
The XSO has the following responsibilities regarding X-ray sources in his/her jurisdiction:
- Hazard evaluation of X-ray sources work area;
- Approval, or recommending for approval, the start of work for new facilities involving the use of X-ray sources, commissioning and decommissioning the X-ray sources;
- Developing and maintaining policies and procedures for engineering and administrative control of X-ray sources hazards. The RSO is also responsible for ensuring that the prescribed controls are in effect;
- Approval of procedures connected with X-ray sources operation that may be subject to administrative and procedural control;
- Inspection of X-ray sources according to the X-ray safety program;
- Recommendation and approval of protective equipment, X-ray sources working area signs and equipment labels;
- Ensuring safe operation through the authority to suspend, restrict or terminate operations; stopping individual/laboratory work when the safety of workers, the public or the environment is at risk; documenting the technical reasons for the above decision, and reporting to the Senior RSO;
- Investigation of the X-ray sources related to incidents and accidents, analysis of the causes, ensuring corrective actions are taken as required;
- Maintenance and up-dating X-ray Safety Database:
- X-ray sources registrations
- Inspection reports
- Training records
- Prepare, maintain and, when necessary, deliver the appropriate X-ray safety training to all categories of personnel according to the X-ray safety program;
- Verifies the quarterly personal dosimeter reports and investigates all the exposure reports that do not appear to be reasonable and appropriate. The results that are over the regulatory limits will be communicated to the Ontario MOL. If a record indicates a value above 0.4 mSv in one quarter and the investigation yields a real result, the XSO will recommend measures to reduce any further exposure;
- Reports on all aspects of the X-ray safety program to Director, Research Safety and Compliance of the Office of Environmental Health and Safety
3.4 Radiation Protection Officer (RPO) for Irradiation on Humans
For X-ray facilities that propose exposure to human subjects (dental, bone density measurements), a Radiation Protection Officer (RPO) who is a member of the Royal College of Dental Surgeons of Ontario shall be appointed as required by the HARP Act. The RPO for a facility has the same responsibilities as the institutional XSO and are also responsible for:
- Ensuring that every X-ray machine operated in the facility is maintained in safe operating condition; and
- Such other matters related to the safe operation of each X-ray machine in the facility as are prescribed by the regulations (Ontario Regulation 663/00 – X-ray Safety Code)
- All appropriate approvals to operate an X-ray source on patients have been obtained from the Ministry of Health (MOH).
- Ensuring workers operating these X-ray sources have adequate training and dosimetry services from the EHS X-ray Safety Officer
3.5 Department Head
The Department Head has the following responsibilities within this program:
- To identify all Permit Holders under his/her authority and ensure that they clearly understand their duties and responsibilities as individuals with principal authority for X-ray sources;
- To ensure that all components of the U of T X-ray Safety Program are implemented in the department.
3.6 Permit Holder (PH)
The PH is in charge of an X-ray source laboratory and/or principal authority for X-ray sources. The PH is an appointed U of T professor.
The PH may delegate some or all of his/her responsibilities to an X-ray sources supervisor. However, the Permit Holder cannot discharge these responsibilities to the X-ray sources supervisor.
The PH has the following responsibilities:
- To register all X-ray sources before use, and to deregister the decommissioned ones with the Radiation Protection Service of the Office of Environmental Health and Safety;
- To identify all X-ray sources, supervisors and workers under his/her authority to the RPS;
- To ensure that X-ray sources supervisors and workers participate in the University’s X-ray safety program training before operating or working in proximity to any X-ray sources;
- To provide and enforce the use of appropriate personal protective equipment when required;
- To provide and enforce the wearing of a personal dosimeter by all X-ray workers when necessary;
- To provide written standard operating procedures (SOPs) for X-ray sources and to ensure that each X-ray source is used only under conditions and in locations that meet the requirements of the SOP(s);
- To ensure that each X-ray sources supervisor/worker is trained in the safe operation of the specific X-ray sources that he/she will operate;
- To ensure that all X-ray machines and X-ray sources are stored securely and safely when not in use so that they are not usable by unauthorized personnel or under unauthorized conditions;
- To allow only trained X-ray sources supervisors/workers to operate or work in proximity of an X-ray source;
- To ensure that all administrative and engineering controls are implemented and followed;
- To correct unsafe conditions on time;
- To ensure that all spectators are properly informed of and protected from potential X-ray sources hazards;
- To cancel X-ray sources supervisor/worker privileges until satisfied that he/she fully meets the requirements of this control program;
- To report immediately known or suspected accidents to the Radiation Protection Service of the Office of Environmental Health & Safety.
3.7 X-ray Supervisor
The X-ray supervisor is an individual who has been delegated supervisory responsibilities for X-ray sources and X-ray workers by the Permit Holder. He/she has the following responsibilities:
- To participate in the University’s X-ray safety program training prior to operating or working in proximity to X-ray sources;
- To be familiar with all operational procedures and specific safety hazards of the X-ray sources that he/she will operate/oversee;
- To operate X-ray sources safely and in a manner consistent with safe X-ray sources practices, requirements and written SOPs;
- To operate X-ray sources only under the conditions authorized by the principal investigator;
- To report all unsafe conditions to the Permit Holder;
- As directed by the Permit Holder, to provide instruction and supervision to X-ray workers;
- As directed by the Permit Holder, to conduct other activities associated with the University’s X-ray safety program;
- To promptly report known or suspected accidents and unsafe conditions to the Permit Holder.
3.8 X-ray Worker
The X-ray worker operates or works in proximity to an X-ray source. He/she has the following responsibilities:
- To participate in the University’s X-ray safety program training before operating or working in proximity to an X-ray source;
- To be familiar with all operational procedures and specific safety hazards of the X-ray sources that he/she will operate;
- To operate X-ray sources safely and in a manner consistent with safe X-ray sources practices, requirements and written SOPs;
- To operate X-ray sources only under the conditions authorized by the X-ray sources supervisor/Permit Holder;
- To report all unsafe conditions to the X-ray sources supervisor/Permit Holder;
- To promptly report known or suspected accidents and unsafe conditions to the X-ray sources supervisor/Permit Holder.
4 Registration of X-ray Sources
4.1 Registering cabinet, mobile and open-beam X-ray sources
There are two primary reasons for preparing and maintaining a record of all X-ray sources. These are:
- To identify areas where X-ray sources are present so that appropriate administrative and engineering controls may be put in place;
- To enable the X-ray sources to be inspected regularly for compliance with the University’s X-ray safety program
The Permit Holder is responsible for the registration of all X-ray sources and the deregistration of decommissioned ones (see X-ray Permit Application form in Appendix 1).
The PH shall request a review of the approval if, after the installation of an X-ray in a permanent location, there is a change in:
- The position or use of the X-ray source;
- The use of the rooms or areas adjacent, horizontally or vertically, to the X-ray source, or
- Any shielding of the X-ray source.
Any of these changes may increase the exposure of faculty, staff, students or visitors.
An X-ray source may be portable or mobile for the purpose if its use. Approval from the MOL must be obtained by RPS for the mobile use of an X-ray source.
The XSO is responsible for the preparation and maintenance of the internal X-ray sources registry and with the MOL.
4.2 Registration of X-ray sources for use on Humans
Any X-ray machine or source used on humans must be registered with the Ministry of Health (MOH) through the facility RPO and meet the requirements outlined by the HARP Act and Regulation 543, including but not limited to:
- Written approval is required prior to machine installation from the MOH (Section 3 of the HARP Act)
- There must be a qualified individual operating the X-ray machine (Section 5 of the HARP Act)
- The irradiation must be prescribed by a qualified individual (Section 6 of the HARP Act)
- There must be a qualified individual designated as the Radiation Protection Officer (RPO) for the facility where the X-ray machine is installed (Section 9 of the HARP Act)
- The X-ray machine must undergo testing immediately after installation and subsequent periodic testing (Section 8 of Reg 543)
4.3 Registration of X-ray Fluorescence (XRF) sources
- The MOL requires certification of all X-ray owners and operators using an XRF analyzer from the Natural Resources Canada (NRCan) National Non-Destructive Testing Certification Body (NDTCB).
- EHS will not submit X-ray applications to the MOL without the necessary certification(s)
- More information regarding the certification process can be found here: https://www.nrcan.gc.ca/science-and-data/non-destructive-testing/about-certification-ndt/apply-xrf-analyzer-operator-certification/19583
5 X-ray Safety Inspections
Periodic inspections of X-ray sources are an integral part of the X-ray safety program; inspections provide some indication as to whether or not these X-ray sources are being operated safely. The X-ray safety inspection checklist is presented in Appendix 3. The PH will be informed about the results of the inspection (a copy of the checklist will be sent to the PH) and of the necessary measures to improve the safe use of the X-ray source.
The XSO is responsible for inspecting all X-ray sources on University of Toronto property on an annual basis in order to maintain compliance with the University’s X-ray safety program. The XSO is also responsible for providing reports to the Radiation Protection Service (EHS) and the UTRPA.
6 Training and Education
All X-ray permit holders, X-ray sources supervisors and X-ray workers must participate in the University’s X-ray safety training before operating or working in the proximity of X-ray machines. The X-ray safety training course is offered online (EHS741) at the following address:
https://ehs.utoronto.ca/training/my-ehs-training/
This training includes the following:
- X-ray basics;
- X-ray hazards, bio-effects;
- Engineering and administrative control measures;
- X-ray safety regulations and U of T X-ray safety program;
- Responsibilities;
- Causes of accidents;
- X-ray accident reports;
- Quiz.
All X-ray supervisors must also be familiar with all standard operating procedures and specific safety hazards of the X-ray machines that they will operate/oversee.
All X-ray workers must also be familiar with all standard operating procedures and specific safety hazards of the X-ray machines that he/she will operate.
To use X-ray mobile equipment, the X-ray worker needs to obtain the appropriate certificate of the Natural Resources Canada (X-Ray Fluorescence Analyzer Operator Certification)
The XSO is responsible for maintaining records of all X-ray supervisors and X-ray workers who have participated in the X-ray safety program training and for notifying Permit Holders of this participation.
All persons using the X-ray machine shall participate every 3 years in the refresher training sessions organized by the RPS. The refresher training (code EHS745) includes:
- X-ray safety updates;
- Changes in X-ray safety legislation;
- Changes in U of T X-ray safety program;
- Responsibilities;
- Results of X-ray safety inspections;
- Quiz.
7 Accident/Incident Reporting and Emergency Response
The University’s health and safety policy requires the reporting of all accidents/incidents, which result in or have the potential to result in a personal injury.
Reporting of accidents involving death, critical injury, lost time or health care is required for employees under the Occupational Health and Safety Act and the Workplace Safety and Insurance Act, while University policy requires the reporting of accidents/incidents involving students and visitors and other persons on university premises.
Therefore, reportable accidents/incidents are those which:
- Result in personal injury (including those requiring first aid) or property damage; or
- Have the potential to result in significant personal injury or property damage even though no injury or damage actually occurred; and
- Occur to any person on university premises; or
- Occur to a university employee during the course of his/her work either on or off university premises.
The Permit Holder is responsible for reporting all accidents/incidents involving X-ray sources:
- For incidents involving employees, the Permit Holder must complete, and sign, the University “Accident/Incident eForm for Employees“
- For incidents involving students, visitors and others, the Permit Holder must complete the “Accident/Incident e Form for Students, Contractors, and Visitors”
Where an X-ray worker has received in one quarter a dose above the annual limit (5 mSv for whole-body exposure of 50 mSv for any individual organ) set out in Column 4 of the Schedule of the Ministry of Labour X-ray Safety R.R.O. 1990, Reg. 861, the XSO will investigate the cause of exposure and will provide a report in writing to the Director of Ministry of Labour, Immigration, Training and Skills Development (MOL) and the Joint Health and Safety Committee of the findings and of the corrective actions taken.
When an accident, failure of any equipment or other incident occurs that may have resulted in a dose received by an X-ray worker is more than the annual limit (50 mSv for whole-body exposure, 150 mSv for the lens of the eye exposure, or 500 mSv for any other individual organ) set out in Column 3 of the Schedule of the Ministry of Labour X-ray Safety R.R.O. 1990, Reg. 861, the PH will notify immediately the Office of Environmental Health and Safety (EHS). EHS will inform, by telephone, or other direct means the Director of Ministry of Labour, Immigration, Training and Skills Development and the Joint Health and Safety Committee. The PH should also send to the EHS a written report of the circumstances of the accident or failure. EHS will send this report to the Director of the Ontario MOL.
All reportable accidents/incidents must be reported to the Office of Environmental Health and Safety within 24 hr so that the appropriate report is filed with the Workplace Safety and Insurance Board.
When a known or suspected accident is reported to the Permit Holder/X-ray sources supervisor or the Office of Environmental Health and Safety, the X-ray sources worker with a suspected injury will be referred to the appropriate University Health Service or hospital
8 Personal Dosimetry
All X-ray workers, supervisors or PHs working with, or within the vicinity of, an open beam X-ray source shall wear whole-body and ring personal dosimeters. If the door of a cabinet X-ray machine is open, the interlock is bypassed for repair, maintenance or beam alignment, the X-ray source must be considered an open beam system.
Dosimeters can be requested from RPS using the “Dosimeter Request Form” available on our website or in Appendix 2. If the X-ray source is enclosed in a cabinet no radiation dosimeter is required. A Canadian Nuclear Safety Commission (CNSC) certified dosimetry service should be used to provide the dosimetry service for the U of T.
The XSO will verify that the dose recorded by the personal dosimeter is reasonable and appropriate in the circumstances and will notify an inspector of the Ontario MOL of any dose that is above the regulatory limits.
The RPS will retain the personal dosimeter records for 3 years. The National Dose Registry of Health Canada keeps lifetime exposure records.
If, when using an X-ray machine for the diagnostic examination of animals, the animals are required to be held by a hand, a protective apron and gloves providing shielding equivalent to at least 0.5 mm of lead shall be worn by the person providing the restraint or support. The person shall wear an extremity dosimeter (ring) under the gloves during the procedure. It is forbidden to hold the film cassette by hand. A record of radiographic exposures, including the date, kilo-voltage, tube current, and duration of each exposure shall be maintained and kept for at least one year.
Each declared X-ray pregnant worker will be provided with a Personal Electronic Dosimeter (PED). The weekly readings of the dosimeter will be communicated to the XSO at the end of each working week. Any unusual reading and anytime alarm sounds will be communicated to the RPS immediately.
9 X-ray Hazard Controls
An important part of the X-ray safety program is the control of the hazards.
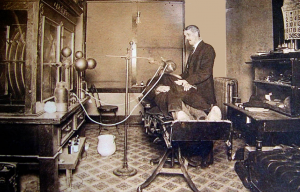
Fig. 9.1: X-ray Safety in the early 1900s
As can be seen in Fig 9.1 at the beginning of the general use of X-ray machines in diagnostics and treatments, there was no control of the x-ray hazards. The physician is exposed to as much radiation as the patient. But since the patient is exposed only when necessary and the physician is exposed with every patient, the total dose received by the physician is much larger. The negative long-term effects of radiation exposure were unknown. A few decades later (the early 1920s) many physicians start dying from cancer. This triggered the creation of the International Commission of Radiation Protection (ICRP).
9.1 X-ray Hazard Assessment
The first step in X-ray hazard control is hazard assessment. The hazard assessment is performed by the X-ray Safety Officer (XSO). The work supervisor (in most university’s laboratories the work supervisor is a University Professor) must inform the XSO by completing and submitting the form from Appendix 1 (see also chapter 4 of this document). The U of T Radiation Protection Service must apply to register the X-ray machine with the Ontario Ministry of Labour, Immigration, Training and Skills Development.
The XSO will visit the laboratory to confirm the information received, estimate the radiation hazards and measure the radiation leaks.
9.1.1 Closed Beam X-ray Machines
An X-ray machine used for sample analysis is considered enclosed in a cabinet if:
- The enclosure provides sufficient shielding to ensure that the radiation exposure at any accessible point of the external surface is under 2.5 microSv/h
- The cabinet’s door is lockable and cannot be opened if the X-ray beam is not
- The cabinet walls cannot be removed without using adequate tools
- The door and any removable part/walls of the enclosure must have interlocks installed
- If the cabinet door or any part of the enclosure are open when the X-ray is not blocked, the interlocks must stop the operation of the X-ray tube
- The X-ray machine must restart from the control panel or computer only when the door or removable walls are closed and interlocks are functional
- The control panel (or the computer used to control the machine) must be situated outside of the cabinet and must indicate the voltage and the current
- The cabinet must have radiation warning labels
- The light indicating that the x-rays are emitted must be visible
9.1.2 Open Beam X-ray Machines
Open beam X-ray machines are usually used in animal facilities, dentistry, and clinics. Sometimes low high voltage and current X-ray machines are used in mobile open beams x-ray machines for sample analysis (geological samples, small animals, etc.) in the field.
If an open beam X-ray machine is used in a permanent location, the entire room will be considered a controlled X-ray zone. Access to the room must be restricted to authorized personnel, the door must have a lock and an interlock. A warning light must indicate the condition of the shutter (open or closed).
9.1.3 Fixed and mobile X-ray Machines
X-ray machines used in a permanent location can be enclosed in a cabinet or open beams. They must be recorded with the Ontario Ministry of Labour, Training and Skills Development as fixed X-ray machines. The mobile X-ray machines have lower high voltage and current and are open beam. They are used to analyse the sample composition in the field.
The mobile X-ray machines are registered with the Ontario MOL as mobile X-ray machines and can be used anywhere in the Ontario province. If a mobile X-ray machine is used outside Ontario it must be registered within the province or territory before can be used in that province or territory.
9.2 Engineering Controls
Engineering controls are physical barriers designed to keep the risks of using X-ray sources under control. When, due to the nature of the device these engineering controls are not applicable, the PH must ensure that equivalent controls are in place. These controls should offer equal or greater protection than the ones described here.
9.2.1 Shielding
To reduce the dose received by X-ray workers according to ALARA and under the permissible limits, structural or another shielding shall be installed as is necessary.
The XSO will assist in calculating the thickness of the shielding for each application when asked by a PH.
If a lead apron and gloves are required when using an X-ray machine the material will provide a shielding equivalent to at least 0.5 mm of lead.
9.2.2 Diaphragms, Cones, Collimators
Diaphragms, cones and adjustable collimators or other suitable devices shall be provided and used as are necessary to limit the dimensions of the useful X-ray beam.
Each port shall be designed in such a way that the X-ray beam can emerge only when a camera or other recording device is in its proper position, wherever applicable.
All unused ports shall be secured in such a way as to prevent inadvertent opening.
9.2.3 Locks, Interlocks
When the radiation exposure in an area may exceed 25 microSv/h access to the area should be controlled by:
- Locks or interlocks if the X-ray source is installed in a permanent location;
- Barriers and X-ray warning signs if the X-ray source is portable or mobile and is being so used;
- A guard or interlock which prevents entry of any part of the body into the primary beam path shall be used, wherever applicable.
When an interlock terminates an exposure, it shall only be possible to restart the exposure from the control panel.
9.2.4 Shutter
A shutter is a mechanical device installed near the exit of the X-ray tube capable of blocking the beam when it is necessary. The shutter may be used in connection with an interlock to stop the beam.
9.3 Administrative and Procedural Controls
Engineering controls must be given primary consideration in instituting a control measure program for limiting access to X-ray sources radiation. If some of these engineering controls are impractical or inadequate, then administrative and procedural controls that provide equivalent protection shall be used.
Administrative and procedural controls are methods or instructions which specify rules, or work practices or both, which implement or supplement engineering controls and which may specify the use of personal protective equipment.
The following are guidelines for the safe use of all X-ray equipment in general:
- The equipment shall be used under the guidance and supervision of a qualified person who is also responsible for the safe use of the equipment.
- X-ray warning signs shall be posted on the doors of all X-ray rooms, and X-ray warning labels shall be affixed to all X-ray equipment.
- All work should be well planned before carrying out an experiment or making an exposure.
- Persons who are classified as X-ray workers shall all wear personal dosimeters, as provided by their respective departments.
- Persons wearing lead aprons should wear their dosimeter under lead aprons to avoid false high readings.
- All equipment capable of producing X-rays shall be lead shielded or installed in a protective lead enclosure. The area in which this equipment is used shall be marked with warning signs to indicate that x-radiation may be present.
- Energized equipment shall not be left unattended in a location with unrestricted access.
- High voltage power supplies using rectifier tubes should be housed in protective lead enclosures.
- A radiation survey of a new or modified X-ray installation and its vicinity shall be carried out before it is put into operation, to ensure compliance with regulatory requirements.
- Protection of staff or students working in areas surrounding an X-ray machine should be achieved by using lead barriers, which absorb the scattered, leakage, or transmitted radiation. The barriers shall be positioned as close as possible to the equipment.
- The primary beam shall be directed towards an unoccupied area (i.e. an area to which access is not permitted) or towards a wall containing adequate shielding. The beam should be well collimated so that it covers only the minimum area necessary for the nature of work being undertaken.
- Protective lead aprons and gloves shall be inspected annually to ensure that they remain in good condition.
- A mobile X-ray machine used routinely in one location should be considered as a permanent installation and be lead or lead equivalent shielded accordingly.
- Before any major change/modification of the approved X-ray installation, or the use of the X-ray machine, which may increase the exposure of the machine user, an application shall be prepared and submitted to the appropriate Ministry through the Radiation Protection for Ministerial re-approval.
- Early submission to the Radiation Protection Service for any new project using an X-ray tube for proposed research or experiment would ensure that any problems could be considered and discussed in advance. A radiation survey shall be carried out before the X-ray work.
- The Radiation Protection Service shall be provided with written notice in advance of any purchase of new X-ray equipment, or the sale, relocation or disposal of an existing X-ray machine or source.
- The X-ray tube shall not be energized during adjustments or repairs or when any protective safety cover is removed.
- No interlock or other safety device shall be deliberately defeated or bypassed.
- Any defect in a piece of X-ray equipment shall be reported immediately to the authority responsible for the radiation safety of the particular equipment and to the Radiation Protection Service.
- Service specialists, such as the manufacturer’s agents will normally carry out repairs, etc. When internal University personnel is used, their competence to control any radiation hazard incidental to the repair procedure, and the use of the repaired equipment, shall be established before initiating the repairs.
9.3.1 Standard Operating Procedures (SOPs)
Standard operating procedures (SOPs) for X-ray machines shall be kept close to the X-ray machine and must always be available as a reference for all X-ray workers; SOPs may include the X-ray sources instruction manual (prepared by the manufacturer) and as appropriate, additional written information to ensure compliance with good work practices and safety.
The SOP must contain information about the X-ray machine (manufacturer, model, serial number, maximum high voltage and current), and the list of authorized personnel.
In addition to the above information, typical examples of SOPs for the X-ray machines used in our university must contain the following information based on the X-ray machine usage.
9.3.1.1 Cabinet X-ray Machine Used for Sample Analysis
- A visual inspection of the signage, functioning of the warning light and integrity of the cabinet must be performed every time before operating the X-ray machine
- Perform the mandatory operation required by the operation manual/instructions given by the manufacturer for starting the X-ray machine
- Prepare and insert the sample in the sample holder
- Close the door and start the measurement
- To change the samples the X-ray machine must be stopped
- After putting the new sample the door must be locked
- At the end of the work the X-ray machine must be closed and the key must be removed. Only authorized personnel must have access to the key
- No radiation badges are required when operating a cabinet analytical X-ray machine
If the interlocks must be bypassed for repair/calibration/alignment the X-ray machine will be considered an open beam X-ray machine. These operations must be performed by a trained X-ray worker wearing a whole-body and a ring radiation dosimeter.
9.3.1.2 Open Beam X-ray Machine Used for Sample Analisis
- Establish the area where the radiation field is above 2.5 microSv/h
- Mark the area with radiation signs and control access to the area by using physical barriers or tape indicating radiation danger. Only persons from the authorized user list are allowed inside the area
- All persons inside the controlled area must wear whole-body radiation dosimeters
- An authorized user must be present when the X-ray is operational
- If the operator must be in an area where the radiation field is above 25 microSv/h, a lead barrier must be used to reduce the exposure under 25 microSv/h
- Perform the mandatory operation required by the operation manual/instructions given by the manufacturer for starting the X-ray machine
- The X-ray emission must be stopped when inserting or changing the sample
- At the end of the work the X-ray machine must be closed and the key must be removed. Only authorized personnel must have access to the key
9.3.1.3 X-ray Machines Used for Animal Diagnosis
- Only persons with adequate X-ray safety and animal safety training are allowed to use X-ray machines on animals
- An X-ray controlled area must be established through walls, doors, physical barriers and marked with radiation warning signs. A warning light must indicate when the X-rays are emitted
- The radiation exposure outside the X-ray controlled area must be under 2.5 microSv/h
- Access to the X-ray controlled area must be permitted only to authorized personnel
- The X-ray machine operator must be outside the X-ray controlled area.
- If possible, the animal must be sedated and no person shall be present in the X-ray controlled area where the operation is performed
- If a person is required to be inside the controlled area to assist the operation by holding the animal, the person must be designated as an X-ray worker, wear a lead apron, lead gloves, and whole-body and ring radiation dosimeters
- Any part of the body of the person must be kept outside the main beam
- The person must never hold the radiography film by hand
- At the end of the work the X-ray machine must be closed and the key must be removed. Only authorized personnel must have access to the key
9.3.1.4 Procedure for Using Dental X-ray Machines
In addition to the relevant precautions set out in previous sections, the following rules shall be observed in using X-ray emitting devices for dental diagnosis:
- In operating an X-ray machine for diagnosis, students or persons in training shall work under the direct supervision of an experienced operator authorized by the person in charge of the department. They shall not be allowed to irradiate patients until they have received sufficient instruction in the precautions necessary for the safe operation of the equipment.
- The X-ray exposure should be controlled only from a lead shielded control booth where the patient can be observed through a viewing window having lead-equivalent thickness conforming to the rest of the shielding.
- Control knobs for adjusting kilovoltage, milliamperage, power-on, or X-ray-on switches shall have their functions clearly and durably labelled.
- All pilot lights, which indicate that the control panel is ready to be energized, shall be ON
- The X-ray tube shall be rigidly fixed and correctly aligned within its tube housing. The tube head shall maintain its exposure position without drift or vibration during the examination.
- Lead-lined localizing collimators or cones shall be used with all dental equipment. Such collimators or cones shall provide the maximum practical field size in conformity with the requirement set by the government, or other regulatory agencies.
- Open-ended cones shall be used for intraoral examinations.
- The equipment shall be provided with an automatic timer, which will terminate the exposure after a preset time or earlier at the discretion of the operator.
- The X-ray tube housing or cone shall not be held by hand during exposure.
- No person other than the intended patient may place any part of his or her body in the direct beam.
- Dental films shall be placed in a fixed position. If the patient is a child or in a weak condition, the film can be held by an accompanying adult who is suitably protected. Under no circumstances may the film be held by a person occupationally exposed to x-radiation.
- Gonadal lead shielding and, when appropriate, thyroid lead shielding shall be provided for all X-ray exposures on children and persons of reproductive age.
- The exposure of the patient during an X-ray examination shall be kept to a minimum necessary to produce satisfactorily diagnostic results.
- An X-ray room in which more than one open X-ray machine is installed shall not be used for more than one X-ray measurement at any one time unless an appropriate barrier has been installed to ensure adequate separation and protection.
- Where more than one tube is controlled by one control panel, dental X-ray equipment shall be designed to facilitate the inclusion of an interlock system such that it is not possible to energize more than one tube at a time and an indicating light will show which tube is connected and is ready to be energized.
To avoid an excessive number of duplicated exposures, the processing of exposed films should be as specified by the X-ray manufacturer.
9.3.1.5 Procedure for Using X-ray Machines on Persons
In addition to the relevant precautions set out in the previous sections, the following rules shall be observed in using radiographic equipment on persons/patients:
- No person shall operate an X-ray machine for the irradiation of a human being unless the operator meets the qualifications and requirements as outlined in the Healing Arts Radiation Protection Act (HARP), and authorized by the individual in charge of the X-ray facility.
- The entrance door to the X-ray room should be kept locked during all exposures.
- X-ray exposure shall be controlled only from the lead shielded control booth.
- X-radiation warning signs forbidding unauthorized use shall be affixed to the control panel of the equipment.
- The beam exposure switch should be of the fail-safe type in which the power is turned off immediately upon release of the switch.
- The total filtration should be permanently installed in the X-ray machine.
- The X-ray tube shall be mounted in lead shielded type housing.
- The equipment shall be provided with collimating devices to keep the size of the primary beam equal or less than the area of the X-ray film selected for each exposure.
- Quality assurance testing for the medical X-ray machine used for patient diagnostic purposes must be carried out following the regulatory requirements set out by the legislation.
9.3.2 X-ray Worker Training
Education and training shall be provided for all X-ray workers (see section 6 of this program). The level of training shall be commensurate with the level of a potential hazard.
9.3.3 Authorized Personnel
X-ray sources shall be operated, maintained or serviced by authorized personnel. Authorization to operate, maintain or service an X-ray machine is given by the PH responsible for the X-ray machine. If authorization is given to an external contractor, the PH must verify the qualifications and the records of X-ray safety training of the contractor and inform the RPS. The XSO will verify the list of the authorized person to confirm that the person/persons have the appropriate training.
9.3.4 X-ray Signs and Warning Signals
Each room that has an X-ray source must have visible signs on all doors indicating that this is an X-ray room.
Each X-ray source shall have the appropriate signs indicating that X-rays are being produced and that moving of the X-ray source to a different room must be communicated to the RPS.
The control panel should indicate when the X-ray machine is producing X-rays.
A warning light shall be mounted near each X-ray machine in such a way as to be visible from any direction from which the X-ray machine can be approached, which indicates when X-rays are being produced.
The status of each shutter, open or closed, shall be indicated at or near the X-ray tube.
In the case of cabinet X-ray equipment, the warning signal should be mounted on or near the cabinet in such a way as to be noticeable from any position from where the cabinet can be opened.
Cabinet X-ray equipment that is intended to allow the entry of a person shall also be provided with:
- Suitable audible or visible warning signals within the cabinet that shall be actuated for at least 10 seconds immediately before the initiation of X-ray production after the closing of any door that is designed to allow human access into the cabinet;
- Suitable audible or visible warning signals within the cabinet that shall activate during X-ray production;
- Effective means within the enclosure to prevent or interrupt the production of X-rays, that cannot be reset from outside the enclosure and that can be reached without having to pass through the primary X-ray beam.
9.4 Personal Protective Equipment
If the X-ray machine is enclosed in a locked cabinet and the radiation leak measurements confirm no radiation dose above the background, the users do not need X-ray protective equipment. They may need the lab coat, gloves and goggles for chemical or biological safety depending on the nature of the samples handled.
For open beam, X-ray machines lead apron and lead gloves may be required to reduce the level of irradiation from direct or scattered X-ray radiation. The personal dosimeters (whole body and ring, if required) will be worn under the lead apron or gloves to eliminate unreasonable dose recordings by the dosimeters.
A protective lead apron and gloves are required to be used when an X-ray machine is used for the diagnostic examination of animals, and the animals are required to be held by a hand. The lead equivalent of the protective apron and gloves must be at least 0.5 mm of lead. The body and the hand of the person must be outside of the X-ray main beam. It is forbidden to hold the X-ray film by hand. Dental patients must be protected by a lead apron. The dental technician using the X-ray dental machine must be outside the room when the X-ray is ON. For more details on the use of lead aprons and gloves see Section 9.3.
A visual inspection of lead aprons and gloves must be performed every time before using them. The visual inspection must identify any tearing or bending of the material. No defective lead apron or gloves will be used.
The XSO must inspect the condition of the personal protective equipment during the X-ray safety inspections (see chapter 5 of this document).
10 Program Audit
The Radiation Protection Service of the Office of Environmental Health & Safety shall audit various components of the X-ray safety program on an annual basis and prepare a report to the UTRPA.
The audit may consist of but is not limited to the following:
- inspections of some X-ray sources facilities for compliance with the University’s X-ray safety program;
- review of training records to confirm that X-ray sources supervisors/workers have had appropriate training to work with X-ray sources;
- review of records vs. inspections to confirm that the registration/ deregistration process is working effectively.
A Joint Health and Safety Committee may, as part of its inspection of the workplace and subject to access control procedures, inspect X-ray sources facilities.
11 X-ray Permit Termination and Disposal of X-ray Machines
Radiation Protection Service must be informed in writing when the installation is no longer to be used for X-ray work.
If the x-ray machine is transferred to a different permit holder or to a different institution the RPS will be informed about the name and address of the new owner.
The following procedure must be followed for the disposal of X-ray equipment.
For the disposal of an X-ray machine, the XSO shall observe the instructions provided by the manufacturer in the product manual or contact the manufacturer for information and guidance. In a case where a manufacturer is no longer in the business of manufacturing, selling or servicing industrial X-ray equipment, the following procedures shall be followed:
- the vacuum in the X-ray tube must be breached;
- the X-ray tube window should be inspected to determine whether or not it contains beryllium, and if it does, special disposal procedures must apply since beryllium presents toxic ingestion or inhalation hazard;
- the transformer oil, if this exists, must be disposed of in accordance with pertinent environmental legislation; and
- the lead must be recycled accordingly
If no other X-ray source remains under the supervision of the PH, the X-ray permit will be archived by the RPS.
12 References
- Occupational Health and Safety Act, X-ray Safety R.R.O. 1990, Regulation 861, Ontario Ministry of Labour
- Healing Arts Radiation Protection Act, Ontario Regulation 663/00 X-ray safety Code Ontario Ministry of Health
Appendix 1 – X-ray Permit Application form
The form to completion can be found in X-Ray Permit Application (PDF).
Appendix 2 – X-ray Training and Personal Dosimetry Form
The form can be found at: Radiation Badge Application Form (PDF)
Appendix 3 – X-ray Safety Inspection Checklist
University of Toronto – Radiation Protection Service |
||||||
Environmental Health and Safety |
||||||
Analytical X-ray Equipment Inspection Report |
||||||
| Permit # | Revision # | |||||
| Principal Investigator | Department | Date | ||||
| Building | Room # | RSO | ||||
| Equipment | ||||||
| Manufacturer | Type | Max kV | ||||
| Model | Serial # | Max mA | ||||
| Code | Description | Y / N | Comments | |||
| A02 | Lab not listed in the appropriate permit | |||||
| A03 | Entry door to lab is not lockable or the lock is not working properly | |||||
| A06 | Lab worker not attached to the corresponding permit | |||||
| A07 | Worker has not taken the required training course | |||||
| A55 | Gas cylinders are not secured at ~ 2/3 their height in an upright position or in an bolted floor mounted apparatus | |||||
| X01 | Current X-ray permit not posted | |||||
| X02 | Drawing approved by MOL not posted | |||||
| X03 | List of authorized X-ray users not posted | |||||
| X04 | Room X-ray sign not posted | |||||
| X05 | X-ray source sign not posted | |||||
| X06 | “Do not move the equipment” sign not posted | |||||
| X07 | UofT Emergency Numbers not posted | |||||
| X08 | Access to X-ray source is not controlled | |||||
| X09 | Unattended labs are not locked | |||||
| X10 | Unattended X-ray sources are not locked | |||||
| X11 | Current SOPs are not posted by the X-ray machine/source | |||||
| X12 | X-ray source not periodically inspected by X-ray supervisor | |||||
| X13 | X-ray source leakage not checked | |||||
| X14 | Appropriate shielding is not available | |||||
| X15 | X-ray machine key control not used | |||||
| X16 | X-ray tube ON warning light not functional | |||||
| X17 | ON/OFF X-ray tube energized sign on control panel not functional | |||||
| X18 | Diaphragms, cones and collimators are not provided if necessary | |||||
| X19 | Primary beam not terminated | |||||
| X20 | Unused port flap shutter not installed | |||||
| X21 | Cabinet/shield/sample interlocks not installed | |||||
| X22 | Interlocks are not functional | |||||
| X23 | Dose rate does exceed 5 μGy/hr (0.5mR/hr) at 5 cm from cabinet | |||||
| X24 | TLD badge not worn if required | |||||
| X25 | Improper TLD storage when not in use | |||||
| X26 | Lead apron or gloves not available or not worn if necessary | |||||
| X27 | UofT X-ray Safety Manual is not available to all users | |||||
| X28 | Principal Investigator or designate not available to supervise | |||||